This report is based on field observations and operational data collected as of March 2025. The report is based on embedding with medical teams and medical evacuations unit in periods between June 2023 and August 2024. Operational security considerations may require adjustments to any implementation strategies. The article is generalized to not reveal sensitive information about specific routes and casualty collection points (CCPs).
The text has been reviewed by medics Sheena, Kirk, Andrew, Max and Anna (last names withheld).
Executive Summary
This report provides an assessment of the current (as of summer 2024) medical evacuation (MEDEVAC) operations in specific regions/sectors of the frontline in Ukraine. Unlike the asymmetrical warfare characteristic of the Global War on Terrorism (GWOT), the conflict in Ukraine represents the first large-scale war – large scale combat operations (LSCO) between near-peer adversaries (NPA) in recent decades, presenting unique challenges for medical operations.
The World Health Organization assessments indicate that over 800 medical facilities and structures in Ukraine have been damaged or destroyed since the full-scale invasion began. The Ukraine Crisis Media Center reports an even higher number—1,100 damaged or destroyed healthcare facilities — creating an unprecedented challenge for healthcare delivery in combat zones. As of May 2025, the Ukrainian Ministry of Health reports as many as 2,300 medical facilities being destroyed since the start of the full-scale war in 2022 (Ministry of Health of Ukraine, 2025) . In 2016, while discussing the Syrian conflict, Michiel Hoffman of Doctors Without Borders expressed concern that attacks on medical facilities and aid workers were becoming increasingly commonplace in warfare and is becoming the “new normal” (Parker, Haldane, & Hodgetts, 2022).
The author has embedded with NGOs that are on contract with the Ukrainian Armed Forces. In addition to contracted NGOs, the armed forces battalions also have their own medical units (Méheut, Konovalova, & Guttenfelder, 2025). Based on field observations, this article focuses on a critical evacuation route between a main hospital facility and forward stabilization points. The findings underscore the significant logistical challenges faced by medical teams operating in this environment and highlight opportunities for operational enhancements to improve patient outcomes and resource utilization.
Operational Framework
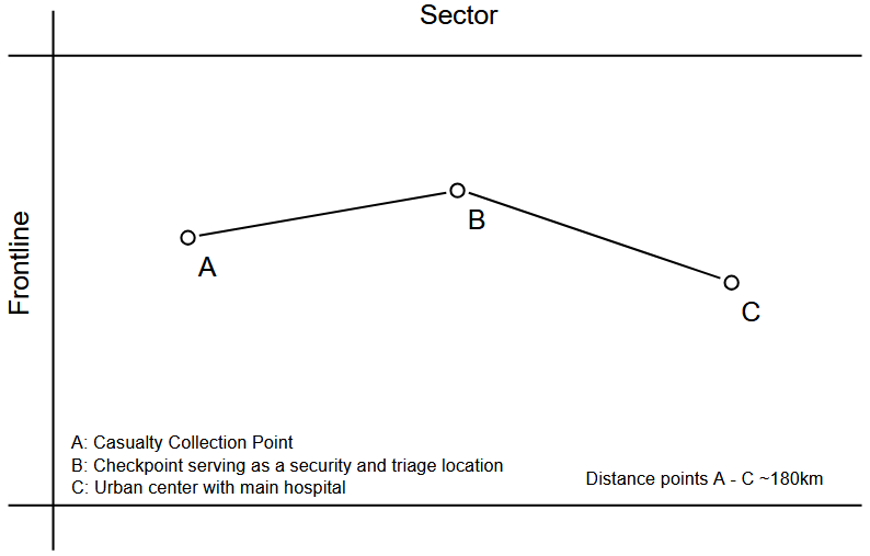
The medical evacuation system of one sector along the frontlines currently operates across a three-point network:
- Point A: CCP and stabilization facility — commonly referred to as stabilization point — located near operational areas.
- Point B: Checkpoint serving as a security and triage location.
- Point C: Urban center with main hospital facilities providing comprehensive medical care.
This triangular evacuation framework necessitates medical teams traversing significant distances under challenging conditions to transport patients requiring urgent care. It's important to note that this system primarily manages combat casualties, which present different clinical challenges and resource demands than civilian medical emergencies. The dynamic battlefield environment introduces additional variables that further complicate medical planning and resource allocation.
Levels of Medical Care
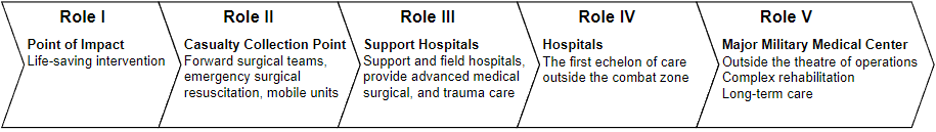
Ukraine began transitioning to NATO medical standards in 2014 as part of broader defense sector reform (Getmachuk, Zarembo, & Fakhurdinova, 2019), and several reforms had been completed by 2019 – before the full scale invasion started in 2022. The military medical system adopted the five-tier JTS structure designed to provide progressively advanced levels of care. However, battlefield realities in the current conflict require flexible adaptation of this framework based on tactical situations, available resources, and enemy threats (Kotwal, 2018) .
In the visited Ukrainian sectors, the medical echelons follow this pattern: Role 1 is the point of impact/injury (POI), Role 2 comprises the CCPs, Role 3 consists of the checkpoints, Role 4 includes urban centers with main hospital facilities, and Role 5 involves MEDEVAC transport to specialized treatment facilities in countries like Norway, Germany, or Austria.
Tactical Adaptation of Signatures
The visual signature of medical operations has undergone complete transformation since the full-scale invasion began. Early imagery showed medical personnel operating in traditional bright ambulances with high-visibility markings and distinctive red EMT gear. Three years into the conflict, this approach has been abandoned due to deliberate targeting of medical assets.
Medical personnel now predominantly wear camouflage patterns indistinguishable from combat units, though some organizations like Doctors Without Borders continue wearing standard EMT clothing as a matter of principle. Ambulances have been repainted with military green or camouflage schemes and operate under camouflage netting when stationary.

Primary medical evacuation vehicles transporting casualties from POI to CCPs now incorporate countermeasures typically reserved for combat vehicles, including IR heat-camouflage and, when resources permit, active defensive systems and anti-drone technologies. These vehicles include both repurposed civilian vehicles (4x4s and SUVs) and U.S.-supplied military vehicles such as Strykers, HMMWVs, and M113 armored personnel carriers.
The tactical adaptation of medical assets reflects a fundamental paradigm shift from protection through identification to protection through concealment, following the "survivability onion" model of layered defense systems — 'Don't be seen, don't be targeted, don't be hit, don't be killled'. This transformation from internationally protected assets to tactically protected assets represents a profound doctrinal shift necessitated by battlefield realities, where adherence to traditional humanitarian conventions now creates vulnerabilities rather than protections (Parker, Haldane, & Hodgetts, 2022).
Information Security Protocols
Operational security extends to patient information handling during the evacuation process. Medical teams typically receive only minimal patient details prior to arrival at pickup locations, with comprehensive information deliberately withheld until the last moment for security reasons. Pre-movement communications commonly use a simplified classification system that provides only the most essential logistical information: "X patients lying down, Y patients sitting, and Z patients that can stand." This necessity for rapid adaptation during patient encounters adds an element of operational stress for medical crews. This uncertainty demands heightened situational awareness and rapid adaptation of treatment approaches based on actual conditions at pickup points—adding significant stress to medical crews and contributing to their cumulative fatigue over time.
This deliberately minimalistic approach to patient information sharing represents an adaptation to communication vulnerabilities and the risk of intercepted transmissions revealing medical movement patterns. By restricting advanced clinical details, the system reduces the operational security risk while still providing evacuation teams with the essential logistical information needed to prepare appropriate transport configurations. This practice reflects the prioritization of movement security over ideal clinical handoff procedures — another example of conventional medical protocols being modified to address battlefield realities.
Casualty Profile Analysis
The Ukrainian conflict presents a distinct casualty profile that requires specialized medical approaches compared to previous combat environments. Historical baseline data from the Global War on Terrorism (GWOT) provides important context for understanding how injury mechanisms have evolved in modern warfare.
The Global Surgical and Medical Support Group (GSMSG) reports a high concentration of blast-related trauma, with approximately 70% of wounds resulting specifically from fragmentation weapons—artillery shells, drone-delivered munitions, and similar explosive devices. (Epstein et al., 2023) As a result of this, casualties often don't arrive with one injury, but a set of wounds (polytrauma) that needs to assessed and treated either concurrently or through localized triage. This represents a further shift away from the penetrating gunshot wounds that were more common during in earlier conflicts.
This concentration of blast and fragmentation injuries creates distinct challenges that directly impact resource requirements throughout the evacuation chain. The nature of these wounds necessitates specialized treatment protocols and equipment configurations that differ significantly from those optimized for conventional gunshot wounds, requiring systematic adaptation of medical support systems.
These casualties typically present with high-energy soft-tissue trauma injuries characterized by:
- Extensive tissue disruption across multiple body regions.
- Complex wound contamination requiring aggressive debridement.
- Higher rates of compartment syndrome requiring fasciotomies.
- Increased need for staged surgical interventions.
- Greater risk of infection and delayed healing.
Analysis of 100 patients treated near front-line positions revealed an average Injury Severity Score (ISS) exceeding 36 from artillery and rocket attacks. This exceptionally high score—where 15 indicates major trauma and 75 is typically fatal—demonstrates the multi-regional nature of these injuries. These types of high ISS values typically indicate serious trauma to multiple body regions, surpassing the severity patterns observed in previous conflicts like Afghanistan (Epstein et al., 2023). These injuries commonly result from a combination of high-velocity penetrating wounds, blast-induced barotrauma, blunt force trauma from explosion displacement, and traumatic brain injuries—particularly during sustained artillery barrages where troops must maintain positions under prolonged fire (following care under fire (CUF) protocols).
An emerging and concerning trend involves patients arriving with respiratory distress and other breathing-related injuries consistent with exposure to gas or chemical weapons. These cases require specialized treatment protocols and present unique diagnostic and management challenges in resource-constrained environments. The presence of these casualties introduces additional complications for medical personnel operating with limited protective equipment and detection capabilities.
The prevalence of these injury patterns necessitates specialized training and equipment focused on managing complex soft-tissue trauma rather than the penetrating injuries that dominated previous conflict medical planning. This shift in injury mechanisms has required adaptive responses across the entire medical support system, from point-of-injury care through definitive surgical management.
CCP Infrastructure Limitations
The operational capacity of Casualty Collection Points is further constrained by significant infrastructure challenges that complicate care delivery. CCPs routinely experience extended periods without reliable utility services, requiring adaptations that impact both clinical capabilities and resource allocation:
- Water Supply Disruptions: Many facilities operate without consistent running water, relying instead on scheduled water tanker deliveries. This necessitates manual water handling protocols where delivered water must be boiled before clinical use—adding labor-intensive steps to already stretched medical workflows. The inconsistent delivery schedule creates planning challenges, as medical teams must maintain sufficient reserves for wound irrigation, sterilization, and basic sanitation while managing uncertain replenishment timelines.

- Electrical Power Contingencies: Grid electricity access is intermittent at best, compelling facilities to depend on generator power for essential functions. The fuel logistics chain required to support these generators introduces another vulnerability point in the medical support system. Limited generator capacity forces medical staff to prioritize power allocation, typically restricting electrical supply to critical care areas, surgical capabilities, and minimal lighting—often leaving administrative, staff support, and secondary clinical areas without power for extended periods.
- Blood Supply Management: The severity and volume of casualties, combined with limited refrigeration capabilities due to power constraints, has led to widespread implementation of "walking blood banks" where soldiers and staff serve as on-the-spot donors for immediate, life-saving transfusions (Gerard et al., 2024). This system addresses both the scarcity of stored blood products and the refrigeration challenges faced by CCPs operating with unreliable power.
These utility challenges create cascading effects throughout the care delivery model. Staff must continually adjust clinical protocols to account for resource fluctuations, implement manual alternatives to equipment typically requiring stable power, and maintain heightened vigilance regarding infection control in sub-optimal sanitation conditions. The time and personnel diverted to managing these infrastructure workarounds diminishes the overall clinical capacity at a time when it is already stretched by high casualty volumes.
CCP Security Protocols
CCPs operate under persistent threat, necessitating the implementation of sophisticated threat detection and response protocols. When imminent danger is identified, all non-essential personnel are rapidly evacuated to hardened shelters known as "Ukrittya." These emergency protocols are triggered by several specific threat indicators:

- Intelligence reports of enemy aircraft takeoff, particularly those known to carry Kinzhal hypersonic missiles or precision-guided glide bombs (KABs/FABs).
- Activation of localized drone detection systems indicating potential incoming aerial reconnaissance or attack platforms.
- Acoustic or electronic detection of incoming artillery rounds.
These reports and detections are fed into automated systems that broadcast alerts over regional and other warning Telegram channels.
While these security measures are essential for protecting personnel, they create operational challenges by forcing medical teams to pause procedures and delay time-sensitive interventions. These sporadic threat-driven interruptions complicate both care delivery and evacuation scheduling, creating yet another challenge in an already complex operational environment.
Key Operational Metrics
Route and Coverage Parameters
- Distance: The critical evacuation route (A → C) spans approximately 180 kilometers
- Transit Time: Each one-way journey requires approximately 2 hours 15 minutes under current conditions.
- Daily Capacity: A single medical team completes 4-6 round trips per 24-hour period depending on conditions. Good conditions allows the route to be driven faster.
- Cumulative Distance: Some medical teams in certain sectors are covering between 1,440-2,160 kilometers daily (4-6 round trips × ~360km per round trip).
Operational Movement Patterns
The checkpoint (Point B) plays a crucial dual role beyond its security function, serving as a strategic buffer zone that enables phased casualty movement during high-risk periods. This buffering mechanism facilitates a key operational adaptation: conducting the most vulnerable evacuations—movements out of forward CCP areas—predominantly during nighttime hours to minimize exposure to enemy drone surveillance and targeting.
Evacuation operations follow a tactical pattern optimized for threat mitigation, with movements occurring during specific time windows that reflect deliberate risk management:
- Early morning movement (05:00-10:00 hours) – Leveraging pre-dawn low visibility
- Mid-day window (10:00-15:00 hours) – Coordinated with hospital surgical team availability.
- Afternoon operations (15:00-20:00 hours) – Depending on whether the evacuation team gets a break or receives another call.
- Evening transport (approximately 20:00 hours) – Initiating night movement cycle
- Pre-dawn final movement (before 06:00 hours) – Completing night operations before daylight.
The checkpoint serves as a relatively safer intermediate holding area where patients can be temporarily staged until daylight movements to the main hospital become feasible, effectively decoupling the evacuation timeline into risk-optimized segments.
In extreme cases, crews have conducted evacuations continuously for over 24 hours (from 05:00 hours one day until 05:00-10:00 hours the next day) before receiving extended rest periods beyond a 15-20 minute break at a local gas station. Weather conditions significantly impact MEDEVAC operations due to drone surveillance and attacks, with clear skies presenting higher threat levels than overcast conditions.
This nighttime movement pattern represents a calculated risk management strategy that extends evacuation timelines to up to 72 hours—a significant deviation from NATO's standard 6-hour protocol, necessitated by battlefield targeting realities.
Route Variations and Crew Management
Evacuation teams also receive calls for shorter-distance movements between single points – particularly Point B to Point C or Point A to Point B. These partial-route movements help maximize resource utilization when full route coverage isn't required, though they can complicate crew scheduling and rest periods if multiple short-distance calls occur in sequence.
Some sectors have implemented efficiency improvements by having medical teams exchange patients at the B-checkpoint, allowing relatively fresh crews to complete the final leg of transport while reducing fatigue and improving response times.
To address the strain on personnel, implementing additional crew rotations would significantly improve operational sustainability. A three-shift system would allow for proper rest periods between deployments, reducing fatigue-related risks and improving overall team effectiveness. Such an enhanced rotation system would not only improve crew alertness and decision-making capabilities but also extend the operational longevity of medical teams working in this high-stress environment.
Vehicle and Maintenance Challenges
The extraordinary operational tempo is imposing severe wear on medical transport vehicles while creating systemic maintenance bottlenecks. Standard ambulances experience transmission failures, suspension damage, and electrical breakdowns at 3-4 times normal rates. Makeshift ambulances (converted civilian vehicles) require complete overhauls at 3,000-4,000 kilometer intervals.
Battery failures are particularly problematic, cascading through electrical systems and disabling critical medical equipment including patient monitors, ventilation equipment, infusion pumps, and emergency airway management devices. Air conditioning failures create dangerous conditions when temperatures fluctuate between +35°C and -18°C along front sectors.
The conflict has created an expertise vacuum in automotive repair, with skilled mechanics recruited into military service. Medical transport units compete for scarce maintenance resources against other essential services. Parts supply chains face weeks-to-months procurement delays, particularly for specialized ambulance systems and European vehicle brands. Import delays are exacerbated by restrictive Polish border policies, adding friction to the medical logistics pipeline.
These combined factors mean minor mechanical failures result in extended asset unavailability, directly impacting operational readiness and requiring higher vehicle redundancy levels rarely available in the current resource-constrained environment.
Medical Supply Uncertainties
Beyond vehicle maintenance challenges, medical NGOs face major uncertainty with their supply inventories. Organizations that rely entirely on donations—either equipment or funding for local purchases—struggle to maintain consistent stock levels month-to-month. This unpredictable supply chain creates serious planning difficulties, as medical teams cannot reliably predict the availability of essential medications, wound care supplies, or specialized equipment for future casualties.
The reliance on donations for supplies creates significant operational risks, further complicating an already complex logistics environment. Medical coordinators must constantly balance immediate usage needs against uncertain future resupply timelines, often resulting in inefficient hoarding behaviors or overly conservative utilization of critical resources. This uncertainty directly impacts treatment decisions and creates additional stress for medical providers who must consider resource availability alongside clinical best practices when determining care plans.
Operational Challenges & Strategic Considerations
The current operational framework faces several critical challenges that necessitate strategic adaptations:
Positioning and Distance Constraints: Russian targeting of medical facilities has forced field hospital relocation from 50-60km to approximately 100km beyond artillery range. Combined with nighttime movement requirements, this extends evacuation timelines to 72 hours versus NATO's 6-hour standard, directly impacting patient outcomes.
Resource and Scalability Limitations: Medical teams spend up to 15 hours daily in transit, creating fatigue issues while reducing direct patient care time. The framework operates with minimal redundancy, creating bottlenecks during mass casualty events when MASCAL protocols must prioritize limited resources using color-coded triage systems.
Staffing Instabilities: Volunteer rotation challenges significantly impact operations, with most volunteers operating on 2-3 week commitments that create substantial administrative overhead and continuity gaps in care delivery.
Strategic Improvements:
- Adaptive Doctrine: Implement modified protocols acknowledging 72-hour evacuation windows with revised triage for extended care scenarios
- Forward Surgical Capabilities: Deploy small, concealed surgical teams between the frontline and safe zones for time-sensitive interventions.
- Enhanced Crew Rotations: Expand successful two-team patient transfer models to full three-team rotations reducing fatigue-induced errors.
- Specialized Training: Recalibrate some of the combat medic training from gunshot wounds to blast/fragmentation injuries (70% of casualties), focusing on complex wound management and debridement techniques.
- Hardened Infrastructure: Invest in partially hardened treatment areas allowing critical care continuation during threat events, plus integrated threat detection systems maximizing procedure completion time.
- Chemical Exposure Protocols: Develop specialized triage and decontamination protocols for documented respiratory injuries consistent with chemical weapons exposure.
Conclusion
The current medical evacuation system demonstrates remarkable adaptation to battlefield realities despite significant deviation from traditional NATO doctrine. The necessity to position field hospitals beyond conventional artillery range (100km rather than 50-60km) and the extended evacuation timelines (up to 72 hours versus the NATO standard 6 hours) represent pragmatic responses to deliberate targeting of medical facilities. While these adaptations have ensured continued medical support capabilities, they have created cascading effects throughout the evacuation chain.
Medical teams have shown considerable resilience in maintaining consistent evacuation cycles across extended distances under high-threat conditions. However, this adapted system operates with minimal redundancy and places extraordinary demands on available medical transport teams. The cumulative effect of these operational adjustments is a MEDEVAC framework that prioritizes medical personnel survival at the necessary cost of delayed definitive care.
Strategic adjustments to the current framework, particularly focusing on distributed forward surgical capabilities and secure transportation corridors, could help bridge the gap between NATO doctrinal standards and current operational realities. Establishing a modified doctrine that acknowledges the 72-hour evacuation timeline as a planned parameter rather than a deviation would enable more effective resource allocation and casualty management protocols.
The evolving threat environment will continue to necessitate creative adaptations of traditional medical support concepts. Continued monitoring of team workload metrics, transportation efficiency, and patient outcomes across extended evacuation timelines is essential to inform future resource allocation decisions and doctrine development.
REFERENCE LIST
Міністерство охорони здоров'я України. (2025, May 8). Понад 2300 об'єктів медичної інфраструктури пошкодила та зруйнувала Росія за час повномасштабної війни. https://moz.gov.ua/uk/ponad-2300-ob-yektiv-medichnoyi-infrastrukturi-poshkodila-ta-zrujnuvala-rosiya-za-chas-povnomasshtabnoyi-vijni
Parker, P., Haldane, A., & Hodgetts, T. (2022, July 27). Dread Cross?. Wavell Room. https://wavellroom.com/2022/07/27/dread-cross/
Méheut, C., Konovalova, O., Guttenfelder, D.. Russia pushes forward around Donetsk as bunkered Ukrainian troops fight on. The New York Times. https://www.nytimes.com/2025/07/07/world/europe/ukraine-war-russia-donetsk.html?smid=url-share
Getmachuk, A., Zarembo, K., & Fakhurdinova, M. (2019). Ukraine and NATO standards: How to hit a “moving target”? New Europe Center.
Joint Chiefs of Staff. (2018). Joint Health Services (Joint Publication 4-02, incorporating Change 1, 28 September 2018). U.S. Department of Defense. https://cdmrp.health.mil/pubs/pdf/Joint%20Health%20Services%20Publication%20JP%204-02.pdf
Kotwal, R. S. (2018, 11. oktober). Department of Defense Joint Trauma System [Presentation]. 30th Annual David Miller Memorial Trauma Symposium, Springfield, MO, USA.
Epstein, A., Lim, R., Johannigman, J., Fox, C. J., Inaba, K., Vercruysse, G. A., Thomas, R. W., Martin, M. J., Konstantyn, G., & Schwaitzberg, S. D. (2023). Putting medical boots on the ground: Lessons from the war in Ukraine and applications for future conflict with near-peer adversaries. Journal of the American College of Surgeons, 237(2), 364–373. https://doi.org/10.1097/XCS.0000000000000707
Gerard, S., Onderková, A., Meoli, M., Leshchenko, Y., Banks, M., Beato, C., Surkov, D., & Quinn, J. (2024, April 9). Large scale combat operations and far forward damage control resuscitation: Observations of Ukraine. Military Medicine Worldwide. Retrieved from https://military-medicine.com/article/4272-large-scale-combat-operations-and-far-forward-damage-control-resuscitation-observations-of-ukraine.html
Photo: Medical Forces of Ukraine Facebook account